ABSTRACT
INTRODUCTION: Trauma to the neck may involve major vascular and aerodigestive structures. While varying diagnostic and treatment algorithms exist for cervical vascular injury, few exist for cervical aerodigestive injury. In addition, combined penetrating and blunt mechanisms of injury to the neck create significant diagnostic and treatment challenges.
CASE REPORT: We present the case of a 39-year old male who sustained cervical and chest stab wounds, requiring emergency thoracostomy tube placement. Computed tomography revealed mediastinal and cervical subcutaneous emphysema but no major aerodigestive injury. The patient underwent operative neck exploration, tracking the caudad direction of the stab wound with negative results. After he developed a cervical wound infection, laryngoscopy revealed posterior tracheal laceration likely secondary to blunt injury, the result of being punched by an assailant wearing a knife ring.
DISCUSSION: Our case reflects layers of complexity: the diagnostic conundrum of combined blunt and penetrating neck injury; unclear guidelines for management of cervical aerodigestive injury; and the limited data available, regarding the rare finding of posterior laryngeal laceration. The direction of the injury combined with the patient’s initial report of only having been stabbed did not warrant operative exploration beyond the knife tract, and imaging, lack of air leak, plus the patient’s respiratory stability dissuaded further workup for tracheobronchial injury.
Posterior laryngeal laceration is most commonly detected by laryngoscopy and has been reported only in the context of blunt trauma. This case also reflects the difficulty in management of violent assault victims where a ring knife has been used.
CONCLUSION: Clinicians treating neck trauma victims should have a high index of clinical suspicion for cervical aerodigestive injury, including rare posterior laryngeal lacerations. In conjunction with advanced technologies and a complete history, cervical injuries can be more effectively and efficiently managed. Guidelines for cervical aerodigestive injury require further development in light of diagnostic complexities.
INTRODUCTION
The assessment and treatment of neck trauma is a complex topic for which various systematic algorithms and expert recommendations are available. 1 – 3 Published data tend to focus on penetrating neck injuries and blunt neck trauma independently, and data commonly address only major vascular injuries. 4 Simultaneous blunt and penetrating injuries sustained within the same anatomical area are rare, and definitive methods for their assessment and management appear to be nonexistent in the literature. When these cases present accompanied by rare injuries such as posterior laryngeal laceration (PLL), they create a clinically challenging dynamic that may increase risk of complications.
More easily visible injuries may obscure the presence of tracheolaryngeal injuries, and tracheolaryngeal injuries can occur in the absence of external signs. Schaefer Fuhrman Classification of Laryngeal Injury Severity assists in evaluation of tracheolaryngeal injury but utilizes primarily endoscopic findings.
Herein, we present a case of combined penetrating and blunt neck trauma, resulting in delayed diagnosis and infectious complications of PLL.
CASE REPORT
A 39 year-old intoxicated male was transported by emergency medical services after reporting being stabbed to the right chest and left neck. Initial airway assessment demonstrated hoarse voice with palpable cervical subcutaneous emphysema associated with a two centimeter transverse stab wound one centimeter superior to the left sternoclavicular junction with obvious tracking toward the mediastinum. The patient had decreased right-sided breath sounds with an approximately five-centimeter transverse sucking chest wound in the midclavicular line at intercostal space five.
A right-sided thoracostomy tube was immediately inserted and evacuated blood and air. The patient then underwent uneventful rapid sequence intubation followed by closure of the chest wound at the skin. Subsequently, the thoracostomy tube revealed no air leak or other evidence of major tracheobronchial injury.
High-resolution contrast computed tomography (CT) of the neck, chest, abdomen and pelvis revealed no major vascular or solid organ injury but did reveal copious cervical and upper mediastinal emphysema (Figure 1) [fig. 1]
and apical right lung laceration—radiography did not localize an aerodigestive injury.
The patient was taken to the operating room where his neck was explored, following and exposing only the entire tract created by the weapon—negative cervical contrast CT and obvious weapon directionality supported a less-invasive and more cosmetic operative approach than formal neck exploration. There was no evidence of tracheobronchial injury. There was no penetration of or air bubbling from the soft tissues deep to the sternum or superior to the cricoid cartilage and no evidence of esophageal leak. A drain was left in the pretracheal space prior to primary, layered closure.
The patient was extubated on postoperative day (POD) one and tolerated clear liquids before progression to a mechanical soft diet with only mild dysphagia. Both chest and neck drains were removed on POD#2. On POD#4, he developed a fever. Repeat chest and neck CT with bronchogram, then contrast esophogram followed by formal swallow study failed to reveal aerodigestive injury. However, a postoperative wound infection was identified, drained and treated with broad-spectrum antibiotics.
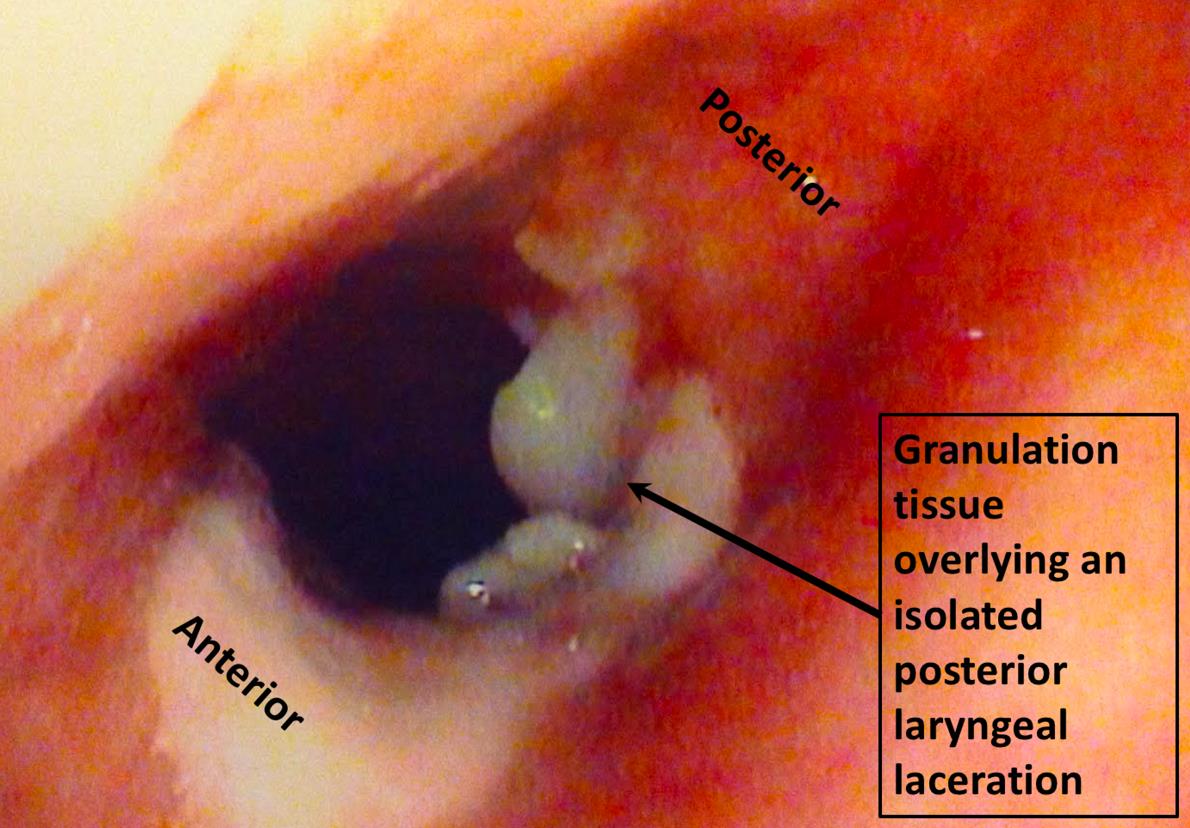
On POD#5, bronchoscopy was performed, revealing a small, healing, isolated posterior laryngeal laceration just below the vocal cords, several centimeters cephalad of the downwardly-angled stab wound (Figure 2). [fig. 2]
Upon further questioning, the patient recalled being punched at least twice in the throat in addition to being stabbed and that the assailant likely was wearing a ring knife.
The patient’s wound infection and leukocytosis resolved without incident. He was discharged home on POD#7 with oral antibiotics and a Penrose drain in the superficial cervical soft tissues. The rest of his course was unremarkable.
DISCUSSION
Our case reflects the complexity of combined penetrating and blunt neck trauma. Our patient suffered both blunt blows and simultaneous stab wounds to the neck and chest likely secondary to ring knife weaponry. Algorithms for managing these combined injuries are insufficient, and development of such algorithms or at least integration of the possibility of blunt trauma to several available penetrating trauma algorithms may inform clinicians treating this variety of injury.
Given the rarity of cervical aerodigestive injury and limitations of CT for its diagnosis, adjunct modalities including fiberoptic imaging or organ-specific contrast studies may be beneficial. An experienced medical team with high index of clinical suspicion for cervical aerodigestive injury is paramount to providing efficient and effective care.
PLL is a rare subset of aerodigestive injury and is only reported as case reports or case series. 5 – 10 Our case of PLL adds to the growing dataset of these injuries, and like most PLLs was the result of blunt trauma and was managed effectively by antibiotics and external drainage.
The easy accessibility of ring knife technology via the internet and the hidden nature of the edged component make ring knives appealing concealed weapons that emergency personnel may encounter more frequently as these weapons proliferate. That this weapon may inflict blunt and penetrating damage simultaneously and within the same anatomical area poses a clinical dilemma such as in our case. Despite clinical, radiographic and operative assessment, our initial care approach failed to account for the blunt component, resulting in soft tissue infection.
Initial assessment failed to discover the Schaefer Fuhrman Class 1 laryngeal injury until after bronchoscopy. Shetty also recounted a case under similar circumstances whereby the initial blunt injury was missed, leading to worsening patient condition. 5 A more detailed classification system including external and radiographic findings for assessment and classification of cervical aerodigestive injuries may more readily inform diagnoses of PLL.
CONCLUSION
Combined blunt and penetrating neck trauma occurs rarely and without established algorithms for assessment or management. Our case reflects the need for more tailored approach to this variety of injury.
FIGURES
REFERENCES
-
Shiroff AM, Gale SC, Martin ND et al. “Penetrating neck trauma: a review of management strategies and discussion of the ‘No Zone’ approach.” Am Surg. 2014; 79:23-30.
-
Sperry JL, Moore EE, Coimbra R et al. “Western Trauma Association critical decisions in trauma: penetrating neck trauma.” J Trauma Acute Care Surg. 2013;75:936-940. doi: 10.1097/TA.0b013e31829e20e3.
-
Feliciano DV. “Penetrating cervical trauma.” World J Surg. 2015;39:1363-1372
-
Franz RW, Willette PA, Wood MJ et al. “A systematic review and meta-analysis of diagnostic screening criteria for blunt cerebrovascular injuries.” J Am Coll Surg. 2012;214:313-327
-
Shetty N, Krishna HM, Varghese E and Gupta A. “Unrecognized blunt tracheal trauma with massive pneumomediastinum and tension pneumothorax.” J Anaesthesiol Clin Pharmacol. 2011;27:406-408
-
Preston T, Fedok FG. “Blunt and penetrating trauma to the larynx and upper airway.” Oper tech otolaryngol. 2007;18:140-143.
-
Sogut O, Cevik M, Boleken ME et al. “Pneumomediastinum and subcutaneous emphysema due to blunt neck injury: A case report and review of the literature.” J Pak Med Assoc. 2011;61:702-704
-
Mussi A, Ambrogi MC, Menconi G et al. “Surgical approaches to membranous tracheal wall lacerations.” J Thorac Cardiovasc Surg. 2000;120:115-118
-
Claes I, Van Schil P, Corthouts B, Jorens PG. “Posterior tracheal wall laceration after blunt neck trauma in children.” Resuscitation. 2004;63:97-102.
-
Shires CB, Preston T, Thompson J. “Pediatric laryngeal trauma: A case series at a tertiary children’s hospital.” Int J Pediatr Otorhinolaryngol. 2011;75:401-408