Introduction
In light of the substantial rise in obesity rates over the past several decades, there has been a surge in bariatric surgeries performed annually. Specifically, the number has increased from around 16,000 in 1990 to around 200,000 in 2020. 1 Although the surgery yields significant weight loss results, it also has potential risks, including rare but serious neurological complications. Prompt diagnosis and treatment of such complications are vital to avoid long-term health effects. We seek to increase awareness of this link by highlighting a case of non-alcoholic Wernicke-Korsakoff syndrome 2 months after gastric sleeve surgery.
Case History
A 48-year-old morbidly obese male with a history of substance use disorder and anxiety presented to the emergency department with a sudden onset of psychotic behavior two months after uncomplicated gastric sleeve surgery. Patient was admitted to the hospital for further evaluation. He had a history of opioid use and was on Suboxone and Klonopin for anxiety. Patient had no history of alcohol use disorder as reported by the patient’s wife and in many previous psychiatric notes. Patient had no relevant psychiatric history and insignificant family history.
Case Presentation
In the ED, the patient’s physical examination and vital signs were unremarkable. The patient’s gait was normal, and he did not exhibit tremors or any signs of ataxia. His pupils were round, equal, and reactive to light. His fundus exam showed sharp discs and no papilledema, and no cranial or carotid bruits. Patient’s mental status was alert and confused, however confabulation was not observed. Patient scored a 21 on the mini-mental state examination, indicating moderate neurocognitive impairment. Cranial nerves II to XII were intact. Motor and sensory exam were normal. The remainder of the physical exam was unremarkable. Delusional thoughts and paranoia were noted. Patient denied suicidal and homicidal thoughts. There was no focal neurological deficit found.
Initial laboratory results were normal. Lab work included arterial blood gas, electrolytes, and a comprehensive metabolic panel that were all within normal limits. Drug and urine toxicology were negative for any illicit substances. Patient’s CT scan was unremarkable, however MRI of the brain demonstrated increased FLAIR signal in the medial thalamic area, peri-mesencephalic area, and periaqueductal area, consistent with Wernicke’s encephalopathy. Initial thiamine level was 81mg (70-180mg being normal). Patient’s lumbar puncture was unremarkable. Patient’s TSH and B12 levels were normal. HIV test and RPR were not performed, as multiple neurological consultations in a local hospital and tertiary care center along with MRI findings were most suggestive on Wernicke encephalopathy.
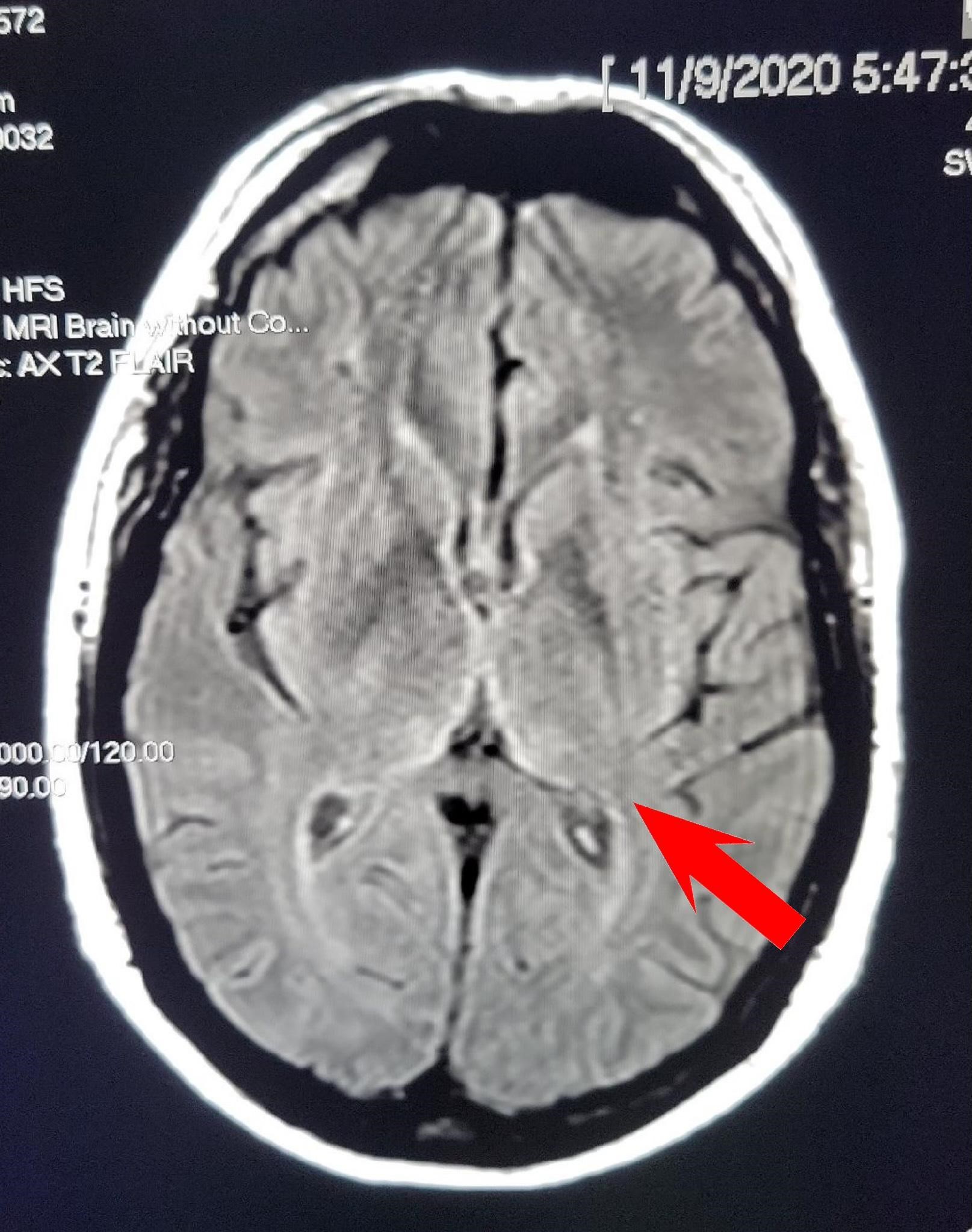
Figure 1: Brain MRI with arrow pointing to increased FLAIR signal at bilateral thalamic region.
Based on clinical and MRI findings, the patient was diagnosed with Wernicke-Korsakoff’s encephalopathy and was discharged on oral thiamine supplements. His cognitive function still continued to decline. Patient admission B1 was 82 mmol/L (70 – 180 mmol/L) and received 100mg B1 orally during the hospital stay and later received 500mg intravenous thiamine supplements daily for 7 days in an outpatient infusion center, however, he did not show improvement. The patient saw a neurologist in a tertiary care center, who confirmed the diagnosis of Wernicke-Korsakoff’s encephalopathy. Patient had an extensive neuropsychological evaluation, which showed circumscribed memory deficit consistent with neurocognitive disorder and behavioral disturbance. Over the course of 2 years, the patient continued to demonstrate a slow decline in cognition, rendering him unable to work in his occupation and he is currently disabled. His most recent follow-up MRI showed improvement in the previously noted thalamic features, and his thiamine levels were found to be normal.
Discussion
There is a well-known link between thiamine deficiency and excessive alcohol consumption, which can lead to Wernicke-Korsakoff Syndrome. That said, thiamine deficiency can also occur in non-alcoholics, however this condition is not as common and is thereby frequently misidentified. 2
This case highlights the importance of routine testing for thiamine levels in the postoperative period of bariatric surgery. Bariatric surgery can lead to the malabsorption and deficiency of essential micronutrients. Given that there are limited endogenous stores of thiamine and most thiamine-rich foods are not typically consumed in adequate amounts post-surgery, the risk of thiamine deficiency is even higher in this population. 3 Thiamine is required for the metabolism of glucose and amino acids, and a lack of it can lead to Wernicke-Korsakoff syndrome, which has two stages. Wernicke’s encephalopathy represents the acute, reversible phase of the disorder. If untreated, it can progress into Korsakoff’s syndrome, which is longer lasting and more disabling. The primary symptoms involve issues in acquiring new information or memories and retrieving old information. 4
If diagnosed early on while still in the Wernicke’s encephalopathy phase, treatment with intravenous and oral supplementation may reverse neurological complications.
It is important to begin intravenous thiamine replacement prior to oral supplements. Evidence-based guidelines show that the most efficient regimen is as follows: 500mg of thiamine three times per day for 2 to 3 days, 250 mg for 3 to 5 days, followed by 100 mg orally three times per day.
2
References
-
Estimate of bariatric surgery numbers, 2011-2020. (2022, June 27). American Society for Metabolic and Bariatric Surgery. https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers
-
Hesami O, Beladimoghaddam N, Assarzadegan F, Kazemi N. Wernicke’s encephalopathy in a non-alcoholic Patient: Difficulties of early diagnosis and treatment. Iran J Neurol. 2012;11:159-61. PMID: 24250887; PMCID: PMC3829265.
-
Albaugh, V. L., Williams, D. B., Aher, C. V., Spann, M. D., & English, W. J. Prevalence of thiamine deficiency is significant in patients undergoing primary bariatric surgery. Surgery for Obesity and Related Diseases, 2021;17:653-658. https://doi.org/10.1016/j.soard.2020.11.032
-
Wernicke-Korsakoff syndrome. (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/wernicke-korsakoff-syndrome
