INTRODUCTION
Brugada Syndrome (BrS) is described as a conduction disorder of the heart with distinct electrocardiographic findings of coved type ST segment elevation in right precordial leads with or without variable degrees of right bundle branch block (RBBB), in the absence of structural abnormalities or ischemia. BrS may manifest with ventricular arrhythmias (leading to syncope and or cardiac arrest) or remain asymptomatic. BrS is largely recognized as the disease of the younger population, most prevalent in third and fourth decades. However, recent case reports highlight that BrS can occur in the elderly population. The diagnosis of BrS in the elderly population requires a high index of suspicion and vigilance. We report 2 cases of BrS in patients in the 7th and 8th decades of life with elusive presentations.
CASE PRESENTATION (1)
A 79-year-old Caucasian male admitted for new onset syncope preceded by dizziness and palpitations. His medical history is pertinent for hypertension, chronic Atrial Fibrillation (AF) on oral anticoagulation and benign prostatic hypertrophy. Family history of cardiac disease or sudden death was absent. Routine home medications included metoprolol, furosemide, warfarin, finasteride, alfuzosin, digoxin and diltiazem. Physical examination was unremarkable.
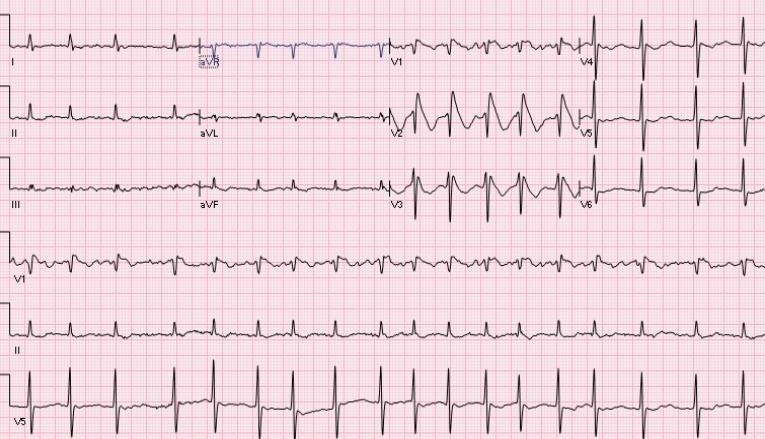
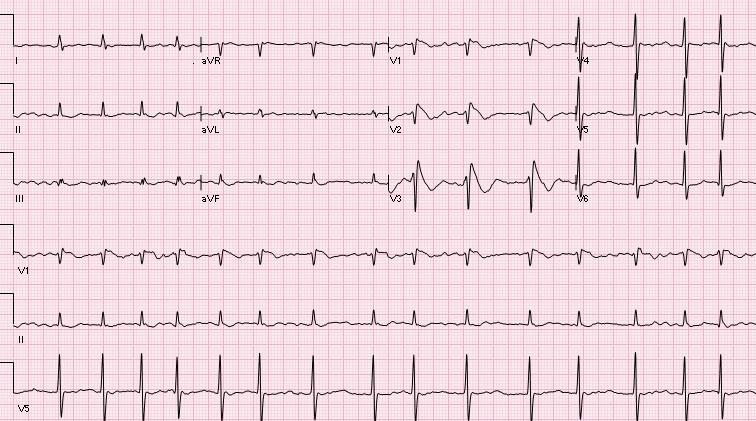
Serial laboratory testing including cardiac biomarkers remained within normal limits. Computed tomography (CT) of head and electroencephalogram results were normal. Trans-thoracic Echocardiography and nuclear stress testing revealed no evidence of structural heart disease or coronary ischemia. On admission, baseline electrocardiogram (ECG) showed AF with incomplete RBBB. Subsequent ECGs revealed spontaneous coving ST segment elevations in V1 through V3 with RBBB, consistent with a Type- 1 Brugada pattern ECG. [fig. 1] , [fig. 2] The patient’s ECG returned to his baseline ECG after 48 hours.
The patient remained asymptomatic and his cardiac biomarkers were within normal limits and for further risk stratification an electrophysiology study was recommended. Programmed electrical stimulation with up to triple extra stimuli from two distinct right ventricular sites produced frequent salvos of non-sustained ventricular tachycardia (VT) but sustained VT or ventricular fibrillation was not induced. Subsequent provocative sodium channel blocker infusion test with procainamide reproduced prototypal BrS pattern ECG changes (coved type ST segment elevation in right precordial leads and RBBB) consistent with a positive response.
CASE PRESENTATION (2)
An 81-year-old Caucasian male patient referred by a local cardiologist for evaluation of recent, multiple episodes of traumatic syncope. His detailed history excluded vaso-vagal and neurologic syncope. His medical history is significant for paroxysmal AF, depression and benign prostatic hypertrophy. He recalled having frequent episodes of syncope and pre-syncope in his third decade of life. Those episodes were never evaluated or treated. Patient’s medications included coumadin, pantoprazole, tamsulosin.
Patient consumed ethanol occasionally, but denied any tobacco use. Family history is significant for sudden death in his father before age 45 years and a brother died of heart disease at age 60.
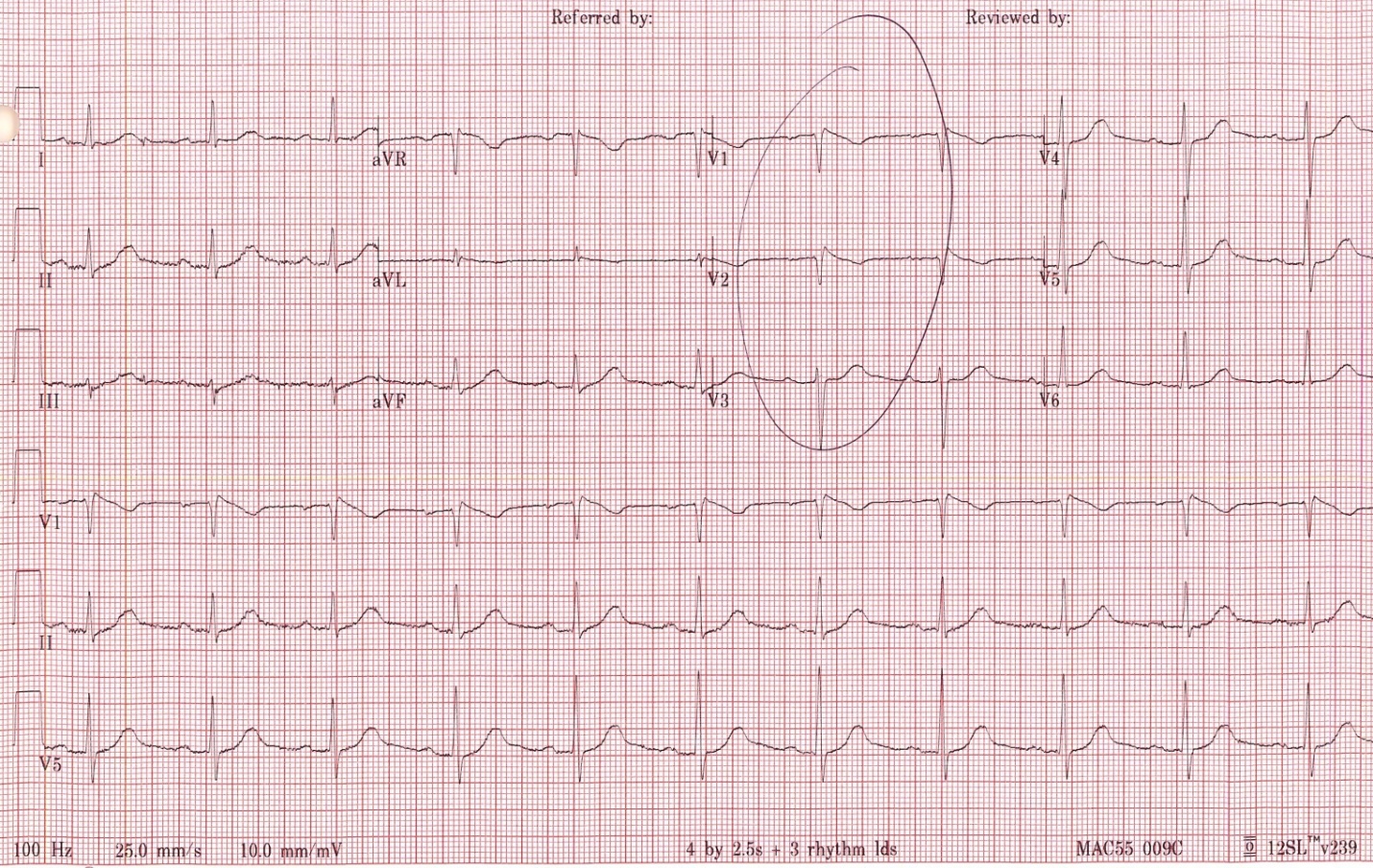
Physical examination was unremarkable and negative for orthostatic hypotension. Hematologic laboratory values, electrolyte levels, cardiac biomarkers for ischemia and B-type natriuretic peptide were with normal range. Initial ECG showed sinus rhythm with prolonged PR interval, normal QT/QTc interval, and variable degrees of right bundle branch block (RBBB), coved type ST elevations in V1-V3 with tallest being 5mm and shortest being 2mm. [fig. 3] The ST elevations were dynamic.
An echocardiogram was performed. The results revealed normal systolic function, wall motion and valvular function. Cardiac catheterization showed non-obstructive coronary artery disease with normal pressures, and left ventricular ejection fraction of 65%.
Head up tilt table test was done and positive for vaso-depressor effect without evidence of chronotrophic incompetence or reproducible syncope. Given the positive family history of sudden cardiac death in first degree male relatives, ECG changes and repeated syncope, we proceeded with electrophysiology study.
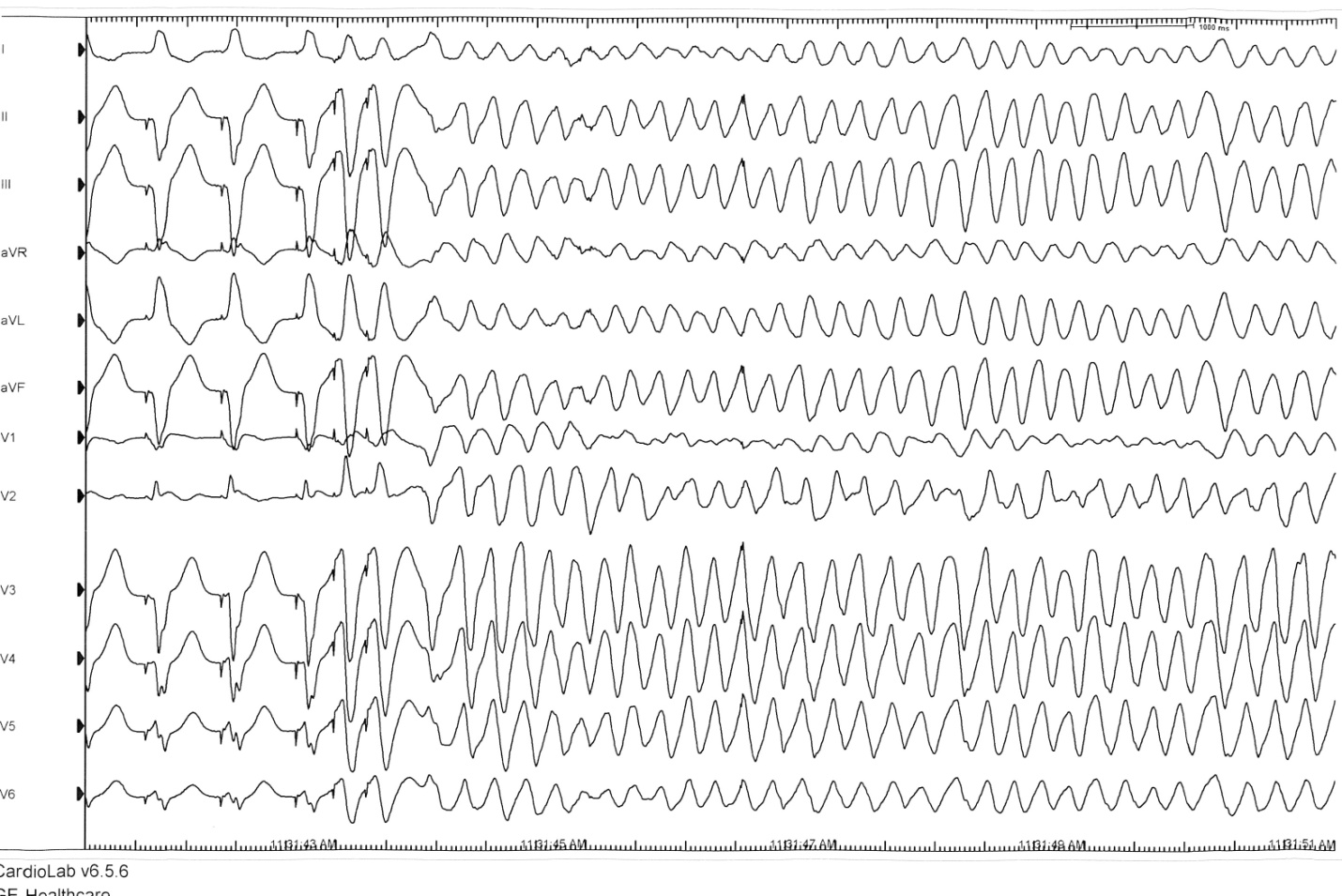
The electrophysiology study revealed normal sinus rhythm with normal sinus node function, normal atrioventricular (AV) node functional testing and no inducible supra-ventricular arrhythmia. H-V conduction was prolonged without evidence of infra-hisian block with physiologic pacing from the high right atrium(hv-interval -126 ms). Ventricular tachycardia was easily induced with double extra-stimuli (600/320/260 ms) from the first right ventricular site. [fig. 4]
Sodium channel provocative testing with procainamide was done and changes are consistent with BrS.
DISCUSSION
The average age at which patients are diagnosed with BrS is 41 years. 1 , 2 BrS rarely presents in the elderly population and it is not well studied in this age group. The clinical presentation, mortality and treatment in the elderly is still unclear. 3
BrS leading to syncope in the elderly has recently been described. In the elderly the mechanism of syncope is often multifactorial. Diagnosis of BrS can easily be missed by 4 less likely age of patient, 5 dynamic, transitory nature of Brugada pattern ECGs, 6 co-existence with other arrhythmias such as AV block and AF, and 1 other more common causes of syncope for their age range. 7 , 8
In a study by Conte et al. elderly patients with BrS were more likely to present with conduction abnormalities on electrocardiogram when compared to younger patients 3 . In addition, patients who were 60 years or older who presented with BrS were also seen to have a prior history of transient atrioventricular block. 3
Due to overlapping manifestation of cardiac channelopathies, presence of atrial arrhythmias may not warrant exclusion of BrS as a possible diagnosis, especially in patients at later years of life. This opens up the contemplation to current clinical age of presentation of BrS. BrS may have a bimodal presentation, the first peak in the 3rd decade and second peak in the 7th-8th decade of life.
We present two cases of patients with syncope as the presenting symptom. A diagnosis of BrS can be made by clinical, electrocardiographic and electrophysiologic findings. BrS is the most likely cause of syncope since all other detectible possibilities of syncope were excluded. Syncope is a common clinical problem with a sharp rise of incidence in the seventh decade of life. Detection of the etiology of syncope has a low yield and cardiac arrhythmia is a common detectable cause of syncope. BrS was first described two decades ago and the knowledge regarding this clinical phenomenon has been expanding. BrS is recognized as a disease of the younger generation by current clinical knowledge.
Initial manifestation of BrS due to electrical vulnerability may manifest at the atrial level with AF instead of ventricular arrhythmias and sudden cardiac death.
This case highlights that BrS should be considered in elderly patients with complete or incomplete RBBB and an unexplained syncope. Atrial Fibrillation happens to be the most common cause of arrhythmia in elderly patients and is also linked to SCNA mutation abnormalities. Prevalence of BrS in elderly may be higher than expected.
FIGURES
REFERENCES
-
Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Giordano U, et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation. 2002;105:1342-7.
-
Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003;108:3092-6.
-
Conte G, Asmundis C, Sieira J, Levinstein M, Chierchia GB, Giovanni G, et al. Clinical characteristics, management, and prognosis of elderly patients with Brugada syndrome. Journal of cardiovascular electrophysiology. 2014;25:514-9.
-
Brugada P, Brugada JJ. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-6
-
Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, et al. Brugada syndrome: report of the second consensus conference. Heart Rhythm. 2005;2:429-40
-
Brugada J, Brugada R, Antzelevitch C, Towbin J, Nademanee K, Brugada P. Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-8.
-
Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, et al. Incidence and prognosis of syncope. N Engl J Med. 2002;347:878-85
-
D’Ascenzo F, Biondi-Zoccai G, Reed MJ, Gabayan GZ, Suzuki M, Costantino G et al. Incidence, etiology and predictors of adverse outcomes in 43,315 patients presenting to the Emergency Department with syncope: An international meta-analysis. Int J Cardiol. 2011;167:57-62