Abstract
Cases of portal vein thrombosis (PVT) are rare and emergent conditions in which there is a complete or partial obstruction of the portal vein. PVT is known to occur in patients with inherited or acquired hypercoagulable states such as malignancy, liver disease, factor V Leiden, and other hypercoagulable disorders. Pro-thrombotic states can also occur in patients undergoing treatment with hormone therapy, such as testosterone replacement therapy (TRT). We aim to bring awareness of the possible complications of TRT, by highlighting a case of severe abdominal pain in the emergency department leading to the rare diagnosis of acute PVT.
Introduction
It is approximated that between 2 to 4 million men in the US have acquired or congenital hypogonadism. 1 In the US, the number of men pursuing TRT use has increased from 1.8 to 4 fold over the past twenty years following an increase in direct-to-consumer advertising and testosterone testing. 2 TRT has benefits in multiple areas of the body including increasing bone density, increasing strength, improving libido, mood, and otherwise unexplained anemia. 3 , 4 , 5 , 6 The possible risks of TRT are continuously being studied, while there is unclear evidence of risk of prostate cancer, there are documented links between TRT and increased coronary artery plaque and erythrocytosis. 7 , 8 , 9 We present here a case of PVT in a patient with intramuscular testosterone replacement therapy to bring awareness to the increasing use of testosterone replacement therapy in older males, and the presentation of an uncommon cause of abdominal pain in the emergency department.
Case Report
A fifty-nine year-old male previously on testosterone replacement therapy presented to the emergency department with severe abdominal pain for five days. For the past 20 months, the patient had received intramuscular injections of testosterone for acquired hypogonadism. The patient’s past medical history included well controlled hyperlipidemia and diabetes mellitus. He had no history of tobacco, alcohol, or drug use. He presented afebrile, normotensive in the emergency room while initial labs showed acute kidney injury BUN 66 mg/dL, Cr 2.7 mg/dL, no anemia with hemoglobin 18.9 g/dL. There was no evidence of cirrhosis showing laboratory values of albumin 2.8 g/dL, AST (aspartate aminotransferase 42.0 U/L, ALT (alanine aminotransferase) 53.0 U/L, alkaline phosphate 53.0 U/L, total bilirubin 0.7, INR (international normalized ratio) 1.19, PT (prothrombin time) 14.5 seconds. Recent outpatient colonoscopy was unremarkable and annual prostate specific antigen (PSA) measurements are within normal range with no suggestion of any underlying malignancy. Initial abdominal computed tomography scan revealed portal vein thrombosis, extending to the superior mesenteric vein and inferior mesenteric vein.
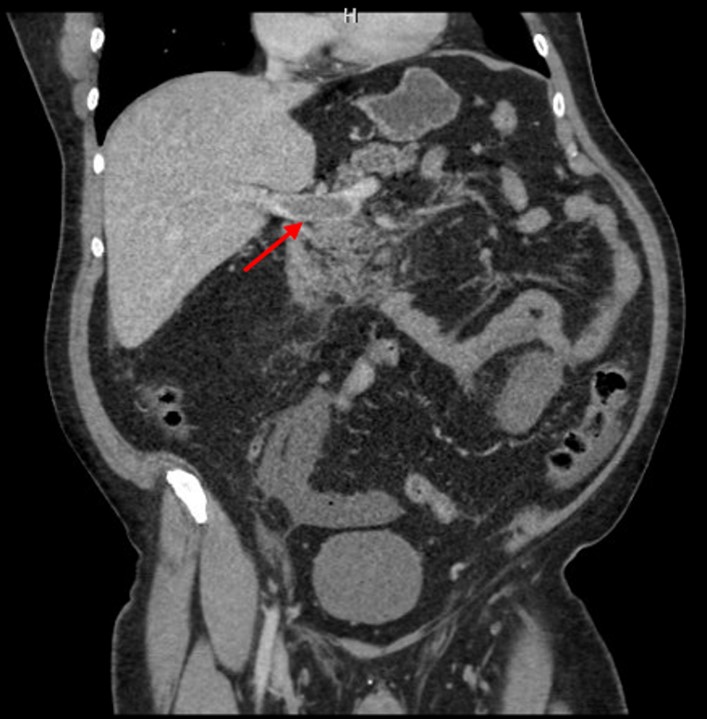
Figure I: Non-contrast CT abdomen with arrow pointing to non-obstructive portal vein thrombosis.
Unfortunately, due to bowel ischemia the patient required aggressive treatment with thrombectomy and a transjugular intrahepatic portosystemic shunt (TIPS) procedure to treat his portal hypertension. He was placed on multiple different IV antibiotics to treat septic shock secondary to bowel obstruction and bacterial invasion through the gut mucosa, known as gut translocation. The patient’s hospital course was also complicated by acute kidney injury, ischemic hepatitis, and respiratory distress requiring intubation. He had hepatic encephalopathy that resolved with lactulose and rifaximin treatment in the hospital setting. The patient was initiated with low molecular weight heparin then transitioned to warfarin. He was then discharged to home with outpatient physical rehabilitation therapy.
Discussion
Our patient represents a rare case of acute PVT in the setting of testosterone therapy treatment. The prevalence of PVT in non-cirrhotic patients is uncertain, while up to 10% of patients with portal hypertension can develop PVT.
10
,
11
Clinical presentations of acute PVT can include sepsis, fever, abdominal pain, rectal bleeding, or abdominal distention. PVT can induce intestinal ischemia which is a surgical emergency. His outcome illustrates several complications of PVT including bowel ischemia, sepsis, hepatic encephalopathy leading to aggressive surgical treatment with transjugular intrahepatic portosystemic shunt (TIPS) procedure.
Emergent imaging with abdominal ultrasound or computed tomography can confirm the diagnosis. Many cases of portal vein thrombosis are treated with therapeutic anticoagulation, mechanical thrombectomy and thrombolytic therapy. It is recommended for acute PVT to treat with six months of anticoagulation and extend the treatment lifelong if there are no underlying hypercoagulable states determined.
17
Anticoagulation is initiated with low molecular weight heparin with later use of oral medications such as a direct-acting oral anticoagulant or warfarin.
18
In our patient’s case, after several months the patient was transitioned to apixaban from warfarin for long term anticoagulation due to his absence of acquired or inherited thrombophilia disorders. He was referred to hematology for workup of a possible underlying thrombophilic disorder.
TRT has been documented to cause erythrocytosis leading to increased blood viscosity, platelet dysfunction, and decreased venous return creating a potential for vascular complications.
7
Several studies have proposed the possible causes of increased erythrocytes, concluding that testosterone may have the ability to suppress hepcidin which controls iron homeostasis, thus creating a potential for an increase in iron absorption and transport, triggering erythropoiesis.
12
,
13
Hughton et al and Ayele et al have investigated the link between venous thromboembolism and testosterone replacement therapy, showing statistically low certainty of association but clinically increased risk is still in question.
14
,
15
More recently, a case-crossover study by Walker et al showed increased short-term risk of venous thromboembolism in association with TRT in men with and without hypogonadism.
16
Thromboembolism caused by TRT was recently studied by Martinez et al in a population based case-control study which concluded the increased risk of thromboembolism was linked to time since initiation of TRT. The study stated that the incidence of venous thromboembolism in patients on TRT is projected to be 10.0 per 10,000 person years within six months of starting TRT treatment with an overall decline in incidence after six months of TRT.
19
With the marketing and sales of TRT increasing each year, prescribers and patients must be made aware of possible adverse side effects of TRT, and these must be further studied.
References
-
Rhoden EL, Morgentaler A. Risks of testosterone-replacement therapy and recommendations for monitoring. N Engl J Med. 2004 Jan 29; 350:482-92.
-
Bandari J, Ayyash OM, Emery SL, Wessel CB, Davies BJ. Marketing and Testosterone Treatment in the USA: A Systematic Review. Eur Urol Focus. 2017 Oct;3:395-402.
-
Yabluchanskiy A, Tsitouras PD. Is Testosterone Replacement Therapy in Older Men Effective and Safe? Drugs & Aging. 2019 Nov;36:981-989.
-
Snyder PJ, Kopperdahl DL, Stephens-Shields AJ, et al. Effect of Testosterone Treatment on Volumetric Bone Density and Strength in Older Men With Low Testosterone: A Controlled Clinical Trial. JAMA Intern Med. 2017;177:471-479.
-
Cunningham GR, Stephens-Shields AJ, Rosen RC, Wang C, Bhasin S, Matsumoto AM, et al. Testosterone Treatment and Sexual Function in Older Men With Low Testosterone Levels. J Clin Endocrinol Metab. 2016 Aug;101:3096-104.
-
Borst SE, Mulligan T. Testosterone replacement therapy for older men. Clin Interv Aging. 2007;2:561-566.
-
Ohlander SJ, Varghese B, Pastuszak AW. Erythrocytosis Following Testosterone Therapy. Sex Med Rev. 2018;6:77-85.
-
Budoff MJ, Ellenberg SS, Lewis CE, Mohler ER 3rd, Wenger NK, Bhasin S, Barrett-Connor E, et al. Testosterone Treatment and Coronary Artery Plaque Volume in Older Men With Low Testosterone. JAMA. 2017 Feb 21;317:708-716.
-
Salter CA, Mulhall JP. Guideline of guidelines: testosterone therapy for testosterone deficiency. BJU Int. 2019 Nov;124:722-729.
-
Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, et al. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004 May;40:736-41.
-
Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006 Apr 7;12:2115-9.
-
Bachman E, Feng R, Travison T, Li M, Olbina G, Ostland V, et al. Testosterone suppresses hepcidin in men: a potential mechanism for testosterone-induced erythrocytosis. J Clin Endocrinol Metab. 2010 Oct;95:4743-7.
-
Guo W, Bachman E, Li M, Roy CN, Blusztajn J, Wong S, et al. Testosterone administration inhibits hepcidin transcription and is associated with increased iron incorporation into red blood cells. Aging Cell. 2013 Apr;12:280-91.
-
Houghton DE, Alsawas M, Barrioneuvo P, Tello M, Farah W, Beuschel B, et al. Testosterone therapy and venous thromboembolism: A systematic review and meta-analysis. Thromb Res. 2018 Dec;172:94-103.
-
Ayele HT, Brunetti VC, Renoux C, Tagalakis V, Filion KB. Testosterone replacement therapy and the risk of venous thromboembolism: A systematic review and meta-analysis of randomized controlled trials. Thromb Res. 2021 Mar;199:123-131.
-
Walker RF, Zakai NA, MacLehose RF, et al. Association of Testosterone Therapy With Risk of Venous Thromboembolism Among Men With and Without Hypogonadism. JAMA Intern Med. 2020;180:190–197.
-
Amitrano L, Guardascione MA, Scaglione M, Pezzullo L, Sangiuliano N, Armellino MF, et al. Prognostic factors in noncirrhotic patients with splanchnic vein thromboses. Am J Gastroenterol. 2007 Nov;102:2464-70. doi: 10.1111/j.1572-0241.2007.01477.x. PMID: 17958760.
-
Primignani M. Portal vein thrombosis, revisited. Dig Liver Dis. 2010 Mar;42:163-70. doi: 10.1016/j.dld.2009.08.003. Epub 2009 Sep 18. PMID: 19766546.
-
Martinez C, Suissa S, Rietbrock S, Katholing A, Freedman B, Cohen A T et al. Testosterone treatment and risk of venous thromboembolism: population based case-control study BMJ 2016; 355 :i5968 doi:10.1136/bmj.i5968
