Diagnosis
Brain abscess rupturing into the lateral ventricle causing meningitis.
Case Report
A 52-year-old male with a past medical history of diabetes mellitus and hypertension, non-compliant with medications, presented to the emergency room complaining of gradual onset of constant headache with neck pain, stiffness and tactile fevers for two days. In addition to photophobia he notes one episode of non-bilious or bloody vomiting. The patient had a history of recent nasal congestion, dry cough and exposure to a sick contact with pneumonia.
On physical exam the patient was found to be drowsy but oriented to person, place and location. His neck was supple, and lungs were clear. Vitals signs in the emergency room: temperature of 100.7 F, pulse 94 bpm, blood pressure 212/108 mmHg, respiration rate of 20 breaths per minute and oxygen saturation of 90% on room air. The remainder of the physical exam was unremarkable. Laboratory results are in Table 1.
Table 1: Laboratory results obtained in the emergency room:
| sodium | 131 mEq/L |
| glucose | 321 mg/dl |
| Carbonate dioxide | 26 mEq/L |
| Lactic acid | 2.3 mmol/L |
| creatinine | 1.0 mg/dl |
| White blood cell count | 17.800 103/ul |
| Platelet | 212 103/ul |
| Chest x-ray | normal |
| HIV | negative |
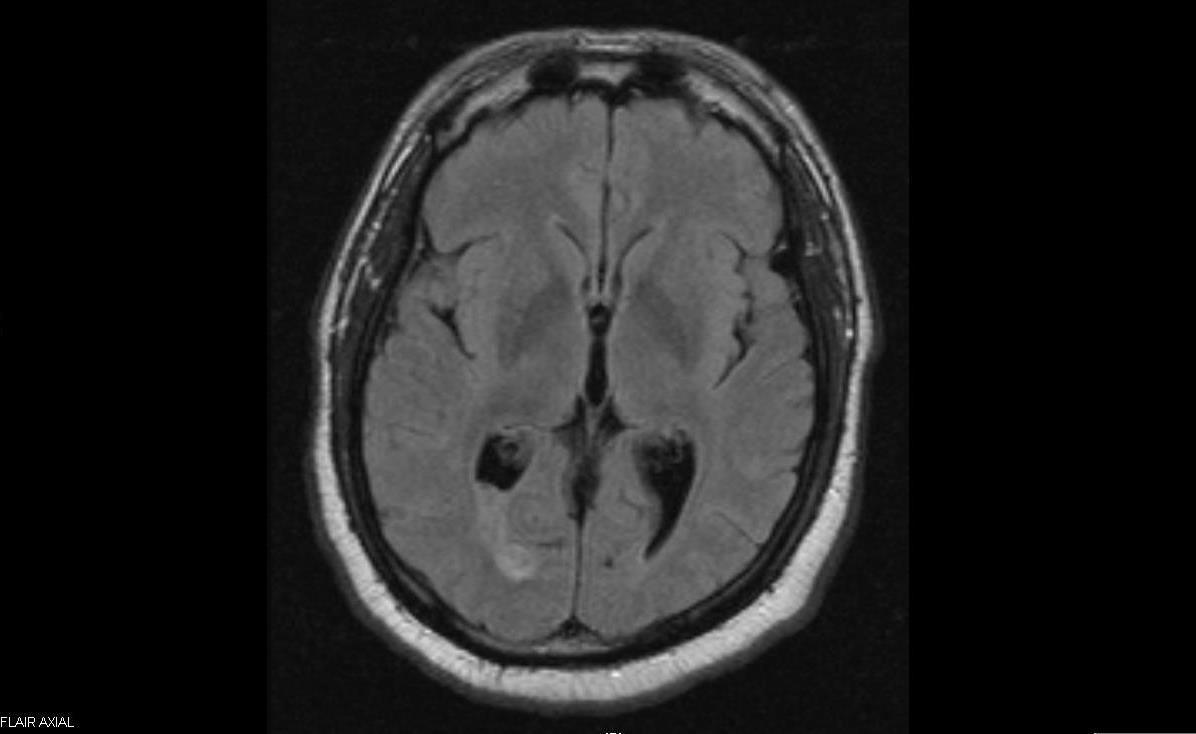
The Patient was placed on droplet isolation. Treatment for presumed meningitis was started with ceftriaxone, ampicillin, vancomycin and dexamethasone. CT scan of the brain without contrast showed no bleed, or intracranial masses [fig. 1] .
Spinal tap results revealed cloudy fluid without xanthochromia, white blood cell 22,225 [/mm3], red blood cells 250 [/mm3], glucose 124, protein 282, neutrophils 71%, monocytes 26, macrophages 3. Gram stain, bacterial antigen, cryptococcal antigen, VDRL and Indian ink were negative.
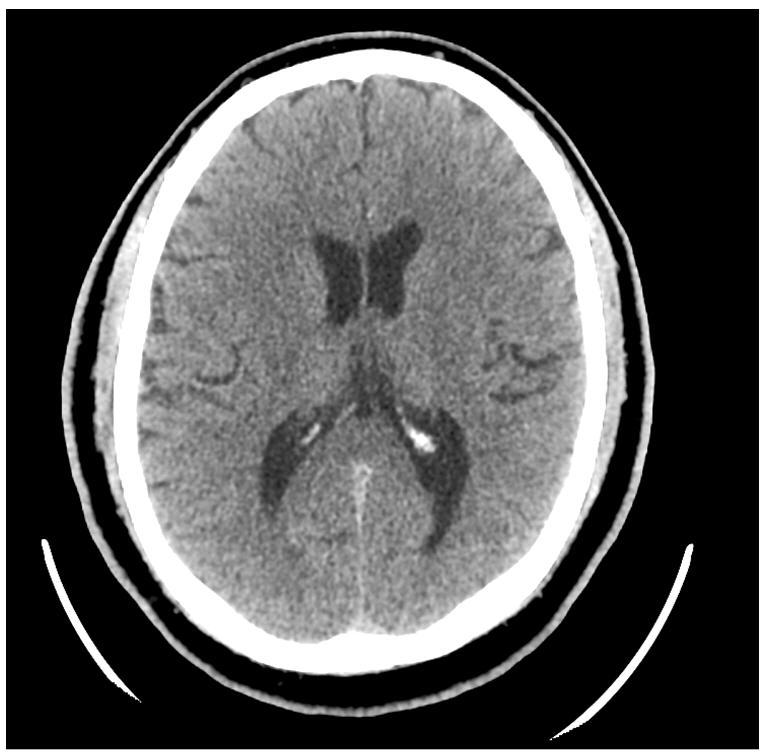
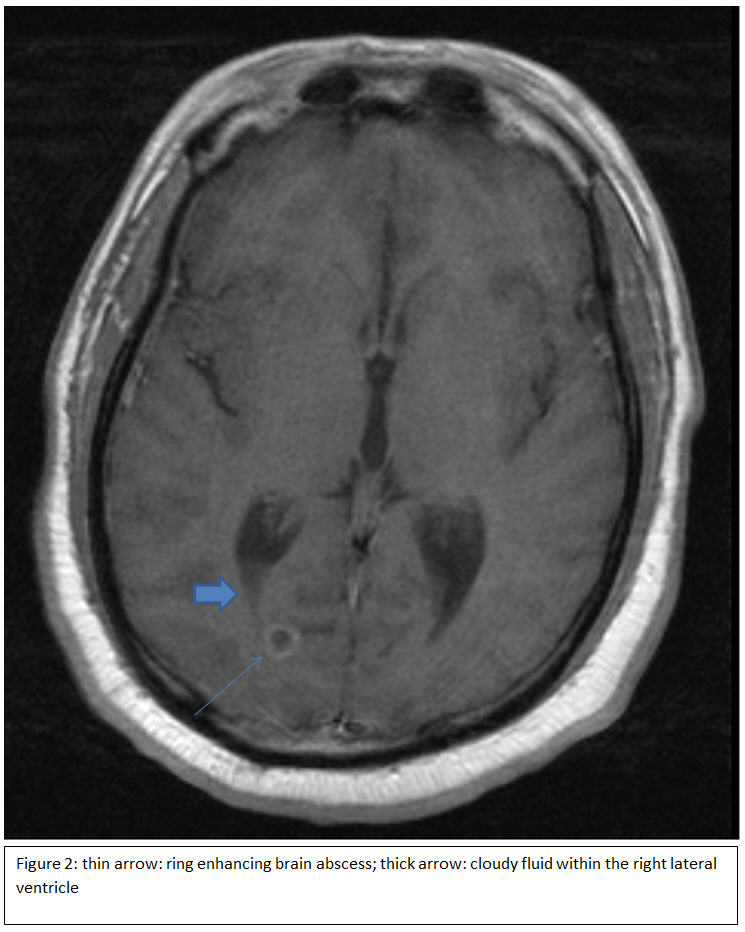
MRI of the brain with and without contrast identified a 9mm ring enhancing structure within the right occipital lobe compatible with brain abscess with direct connection to the right lateral ventricle. [fig. 2] [fig. 3] Metronidazole was added for treatment of brain abscess. Ampicillin was discontinued. Patient’s mental status returned to baseline 24 hours on antibiotic treatment.
On day 4, results from spinal fluid tuberculosis polymerase chain reaction and viral encephalitis panel sent to NYSDOH were negative. Spinal fluid cultures were negative. One blood culture set was positive for propionibacterium acnes. Vancomycin was discontinued.
An MRI obtained six weeks into treatment showed a smaller ring enhancing lesion measuring 3 mm along with enhancement within and adjacent to the atrium of the right lateral ventricle. [fig. 4] The patient was treated for an additional two weeks. Repeat MRI after 8 weeks of treatment showed resolution of the abscess and decreased inflammation of the posterior horn of the right lateral ventricle. [fig. 5] The patient was seen in clinic 6 weeks after therapy. He remained asymptomatic.
Discussion
Brain abscess classically presents with headache, mental status changes, fever and focal neurologic deficit and less commonly with nausea, vomiting, seizures and nuchal rigidity. The location of the brain abscess will also determine the clinical presentation. Brain abscess occurs either by bacteremia with seeding of the brain, by extension from a local infection (dental, sinuses, ears etc.) or from trauma. Most ruptured brain abscesses are located medial to the ventricles, as the capsule surrounding the abscess is less well formed on that side. 1
Streptococcus, Staphylococcus and anaerobes are the most common pathogens. The mortality from brain abscesses decreased significantly with the advent of brain imaging 2 with CT and then MRI and with improved antibiotics that penetrated into the brain and spinal fluid. In a review of brain abscess in 1997 the mortality was reported greater than 80%. 3 In two more recent studies 2 of 12 patients with definite ruptured brain abscesses died. 1 4
The sudden onset of headaches and the high CSF pleocytosis is a clue to a ruptured a brain abscess. Our patient had over 22,000 WBC/mm 3 in the CSF which is higher than the most recent published cases (range from 311 to 10,200 WBC/ul). 1 4
Intraventricular rupture of a brain abscess is a rare event associated with high morbidity and mortality which has improved with better brain imaging. White blood cells in the CSF after rupture can be very elevated and a clue to a ruptured brain abscess.
Figures
References
-
Ferre C, Ariza J, Viladrich PF, Acebes JJ, Tubau F, Lopez L, et al. Brain Abscess Rupturing into the Ventricles or Subarachnoid Space. The American journal of medicine 1999;106:254-257.
-
Zeidman, SM, Geisler FH, Olivi A. Intraventricular rupture of a purulent brain abscess: case report. Neurosurgery 1995;36:189-93.
-
Mathisen GE, Johnson JP. Brain abscess. Clin Infect Dis. 1997;25:763– 81.
-
Karma, P, Vatsal DK, Husain M, Pradhan S, Venkatesh S. MRI demonstration of unsuspected intraventricular rupture of pyogenic cerebral abscesses in patients being treated for meningitis. Neuroradiology 2002;44:114-117.