ABSTRACT
Paraneoplastic cerebellar degeneration is a rare neurological complication triggered by certain underlying malignancies secondary to antibodies against cerebellar antigens. We describe the case of a 71-year-old female who presented with vertigo and ataxic gait. Initial imaging reported schwannoma, but it did not explain the reason for vertigo. Initial lab investigations and MRI Brain were unremarkable. Full body CT scan revealed a large heterogenous pelvic mass. Paraneoplastic panel was positive for anti-Yo antibodies. The patient underwent treatment for her ovarian cancer with surgery and chemotherapy. She had some improvement in her neurological symptoms.
INTRODUCTION
Paraneoplastic cerebellar degeneration is a constellation of neurological symptoms arising from tumor induced autoimmunity against cerebellar antigens. 1 The development of cerebellar dysfunction symptoms without any intracranial space occupying lesion usually points towards an underlying malignancy causing paraneoplastic symptoms. 1 This association between cancer and cerebellar symptoms was first reported in 1949 by Guichard and Vignon. 2 It was later confirmed in 1976 when more cases were identified. 1 , 3 Malignancies involving lung, breast, ovary, fallopian tubes, and Hodgkin’s lymphoma have associated with this paraneoplastic process. 1 Interestingly, each tumor shows a different antibody against cerebellar antigens. For example, anti-Hu antibodies are associated with small cell carcinoma of the lung, anti-Ri antibody is associated with breast and gynecological cancer, and anti-Yu antibody is almost always associated with gynecological cancers such as ovarian cancer. 4 There are about thirty antibodies associated with paraneoplastic cerebellar degeneration. 1
A diagnostic criterion has been developed for paraneoplastic cerebellar degeneration based on guidelines from the paraneoplastic neurological syndrome EuroNetwork in 2004. 1 The diagnostic criteria require the development in less than 12 weeks of cerebellar symptoms, no MRI evidence of cerebellar atrophy other than age related changes, and the development of cancer within five years of neurological symptoms along with onconeural antibody. 1 , 2
CASE PRESENTATION
We report a case of a previously healthy 71-year-old woman who noted three weeks of severe vertigo, not responding to meclizine. Evaluation by otolaryngology and neurology revealed rotatory nystagmus. Initial MRI reported left sided schwannoma and age-related changes. [fig. 1] Neurosurgical team recommended no surgical intervention. Patient returned to the hospital complaining of severe worsening balance and gait disturbance along with speech difficulties. Upon examination, patient was found to have a broad based gait, nystagmus, abnormal finger nose test on the right side, and dysarthria. She denied having any difficulties with swallowing, or pain anywhere. Her past medical history included hyperlipidemia, osteoporosis, and anxiety. Past surgical history was significant for hysterectomy. Patient had no significant family history. She never smoked, was an occasional drinker of alcohol and denied illicit drug use. She was living by herself and had not been able to perform activities of daily living for the prior three weeks.
INVESTIGATIONS
Her work up included a negative CTA Brain and no signs of anemia, leukocytosis, or renal dysfunction. To total body CT was performed because of the underlying suspicion of malignancy. It revealed a large 3.5 x 4.5 cm mass along the right pelvic wall likely arising from the right ovary. [fig. 2] Ca-125 was elevated, 40 units/ml.
The patient was discharged to a skilled nursing rehab with outpatient follow-up with neurology and Gynecology-Oncology. Her ataxia and dysarthria worsened in the following weeks. The paraneoplastic panel showed elevated titers for anti-Yo antibody, also called anti-Purkinje cell cytoplasmic antibody. It is responsible for causing Purkinje cell death resulting in cerebellar degeneration.
Patient underwent a bilateral salpingo-oopherecomy procedure and the histopathology was positive for high grade papillary serous carcinoma involving both ovaries and fallopian tubes, with malignancy noted in the peritoneal fluid (FIGO Stage IIB). [fig. 3] She later underwent chemotherapy with taxol and carboplatin. She did well with the first two cycles of chemotherapy. Her neurological symptoms showed some improvement in terms of speech and gait, but she continued to have weakness in her lower extremities. She is currently undergoing physiotherapy, speech therapy, and chemotherapy. The patient’s neurologic status remained unchanged eight months later.
DISCUSSION
Paraneoplastic cerebellar degeneration refers to neurological disorder from autoimmunity against cerebellar antigens. 5 These autoantibodies are induced by an underlying malignancy, likely from breast, ovary, fallopian tube or lung. 1 Ovarian cancer sometimes causes the formation of anti-Yo antibody, a paraneoplastic antibody that is directed against the cytoplasmic antigen called cerebellar-degeneration related protein 2 (CDR2) which has been detected in the tumor and also in the central nervous system. 5 The antibody was first described by Greenlee and Brashear in 1983. 2 It is an IgG antibody, present in high titers in serum and CSF during the paraneoplastic syndrome. The exact mechanism of the antibody causing Purkinje cell death is not clear. 1 It is postulated that antibodies uses both humoral and cytotoxic T-cell response, incorporating CD8+ cells in the death of Purkinje cells of the cerebellum. 1
The prevalence of anti-Yo antibody is very low. 1 A study has reported about 2.3% patients out of 557 with ovarian cancer and 1.6% out of 253 patients with breast cancer were found positive for anti-Yo antibody. 6 Out of those who tested positive, only 12% were found to have paraneoplastic cerebellar degeneration. 6
Ovarian cancer presenting as ataxia and speech difficulty due to underlying cerebellar degeneration has not been widely reported in the literature. 5 Greenlee and Brashear reported two cases in their case report that led to the identification of anti-Yo antibodies causing cerebellar dysfunction. 2 Another case was recently reported by Sharma et al, who described a case of a 61-year-old female presented with abdominal distention, vertigo and slurring of speech. 5 Patient was found to have a large pelvic mass arising from the left ovary, and MRI brain reported age related changes only. Her paraneoplastic panel was positive for anti-Yo antibody and she was found to have high-grade serous adenocarcinoma of the left ovary. 5
There are several case reports in the literature on paraneoplastic cerebellar degeneration syndromes secondary to different underlying solid organ and hematological malignancies. A case of a 65-year-old female presenting with ataxia has been reported by Campero et al. 4 Patient was found to have positive anti-Yo antibodies and was later diagnosed with fallopian tube adenocarcinoma. 4 Martin et al described the case of a rare anti-Yo mediated paraneoplastic syndrome in a patient presented with diplopia, dysarthria and nystagmus. 7 The patient was also found to have pseudobulbar affect. She was diagnosed with Stage III Breast cancer and showed significant improvement in her neurological symptoms after surgery and chemotherapy for underlying malignancy was administered. 7 Another rare case of paraneoplastic syndrome was reported by Zhu et al. 8 the patient in the report was a 68-year-old male with history of urothelial carcinoma of the urinary bladder, who experienced persistent cerebellar ataxia. 8 On further evaluation, the patient was found to have bladder cancer recurrence (high-grade urothelial carcinoma with squamous differentiation) few months after the primary tumor excision. However, antitumor antibodies were not detected in the case, but patient’s neurological symptoms showed dramatic improvement after radical cystectomy was performed for tumor recurrence in the urinary bladder. 8
Treatment of paraneoplastic cerebellar degeneration with immunoglobulins and anti-cytotoxic T lymphocyte agent is under debate. 1 , 9 Recent guidelines by the Agency of Healthcare Research and Quality (AHRQ) recommend early anti-tumor therapy for the stabilization of para-neoplastic cerebellar degeneration in cancer patients. 10
FIGURES
-
Figure 1
There are a few scattered foci of T2 FLAIR hyperintensity involving the periventricular and subcortical white matter, likely represents chronic microangiopathic
changes.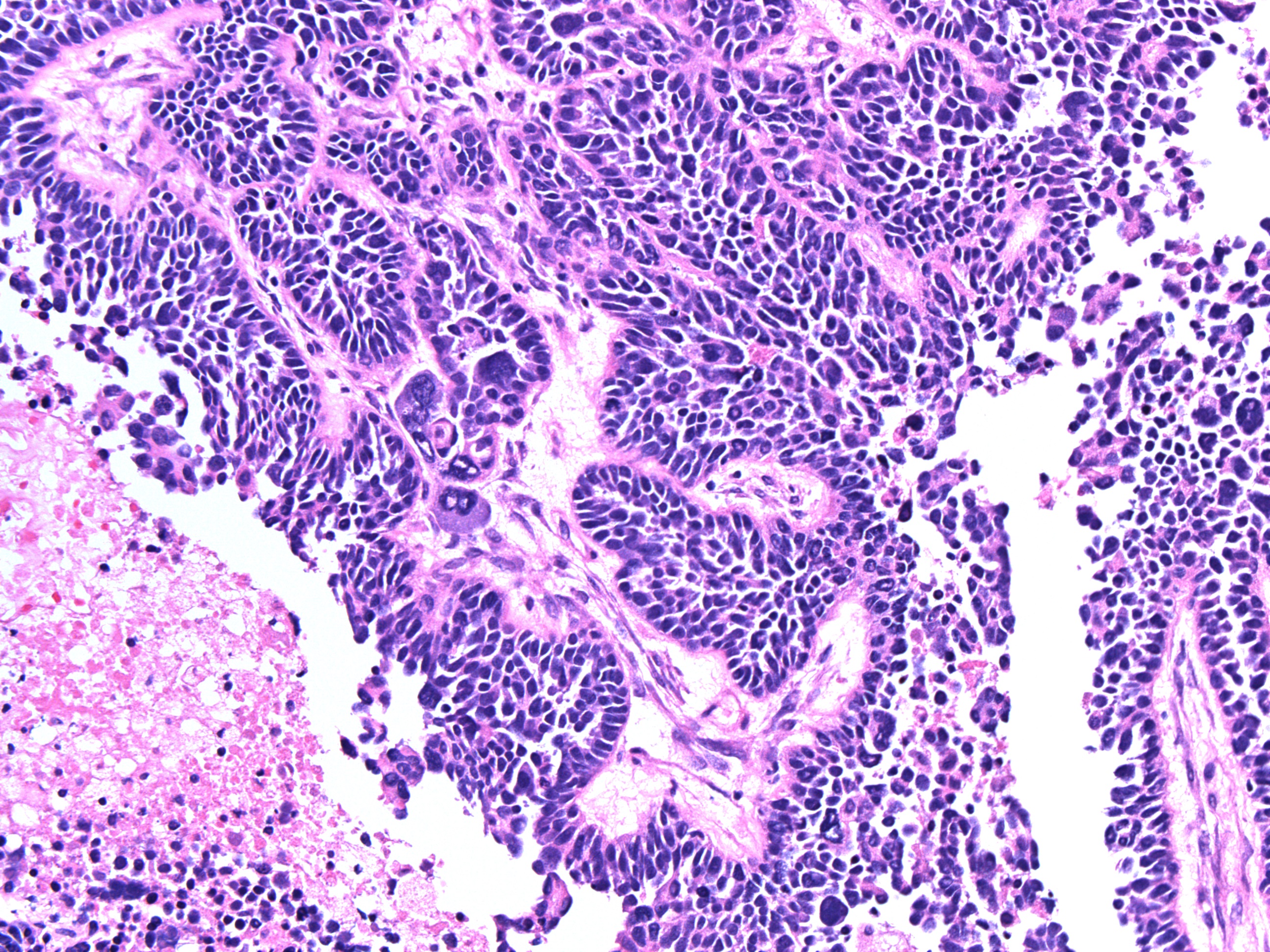
-
Figure 2
A 3.5 x 4.5 cm heterogenous mass along the right pelvic sidewall concerning for malignancy.
-
Figure 3
H&E X 200. High grade papillary serous carcinoma involving the ovary. The tumor cells are pleomorphic with hyperchromatic nuclei and scant amphophilic cytoplasm forming papillary structures.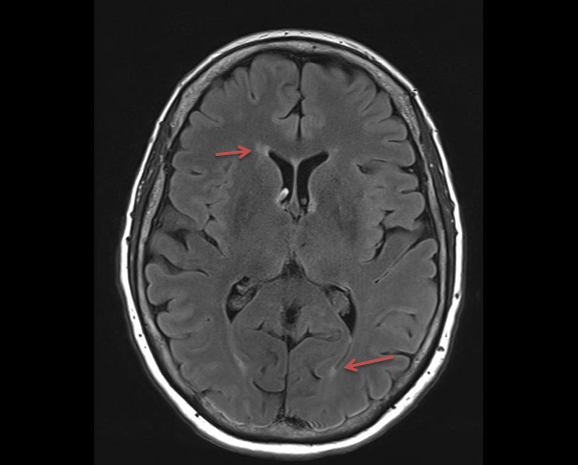
REFERENCES
-
Venkatraman A, Opal P. Paraneoplastic cerebellar degeneration with anti-Yo antibodies- a review. Ann Clin Trans Neurol 2006;3:655-63
-
Greenlee JE, Brashear H. Antibodies to cerebellar purkinje cells in patients with paraneoplastic cerebellar degeneration and ovarian carcinoma. Annals of neurology 1983;14:609-613.
-
Trotter JL, Hendin BA, Osterland CK. Cerebellar degeneration with Hodgkin disease. An immunological study. Arch Neurol 1976;33:660-661
-
Campero M, Selman AE. Paraneoplastic cerebellar degeneration in a patient with primary fallopian tube adenocarcinoma. A case report and brief review. Gyn Onc reports 2017;20:90-92
-
Sharma R, Radhakrishnan G, Radhika AG, Singla A. Paraneoplastic cerebellar degeneration- a rare case of ovarian malignancy. J Obs gynecol India 2016;66:S686-89
-
Monstad SE, Storstein A, Dorum A, et al. Yo antibodies in ovarian and breast cancer patients detected by a sensitive immunoprecipitation technique. Clin Exp Immunol 2006;144:53-58
-
Martin AN, Dillon PM, Jones DE, et al. Anti-Yo mediated paraneoplastic cerebellar degeneration associated with pseudobulbar affect in a patient with breast cancer. Case reports in Oncol Med 2017. https://doi.org/10.1155/2017/8120689
-
Zhu Y, Chen S, Chen S, et al. An uncommon manifestation of paraneoplastic cerebellar degeneration in a patient with high grade urithelial carcinoma with squamous differentiation: a case report and literature review. BMC Cancer 2016;16:234.
-
Albert ML, Austin LM, Darnell RB. Detection and treatment of activated T cells in the cerebrospinal fluid of patients with paraneoplastic cerebellar degeneration. Ann Neurol 2000;47:9-17
-
Paraneoplastic Neurological Syndromes. National guideline clearinghouse: Agency for Healthcare Research and Quality. https://www.guideline.gov/content.aspx?id=34906. Accessed May 01, 2017.
